Blog
ImpeTus
Official blog from Imperetus.
The company transforming how the MedTech world does business.

By Colette Hamilton
•
06 Dec, 2022
As the global incidence and prevalence of PD are expected to rise, doubling between 2005 and 2030, the shortage of neurologists is predicted to increase as well, widening the gap between those in need of specialized PD care and those providing it. A digital monitoring and telemedicine system could be the only affordable way of closing the gap between existing practice, guidelines for good practice and health needs.
By Charles Daniel McDonald
•
06 Dec, 2022
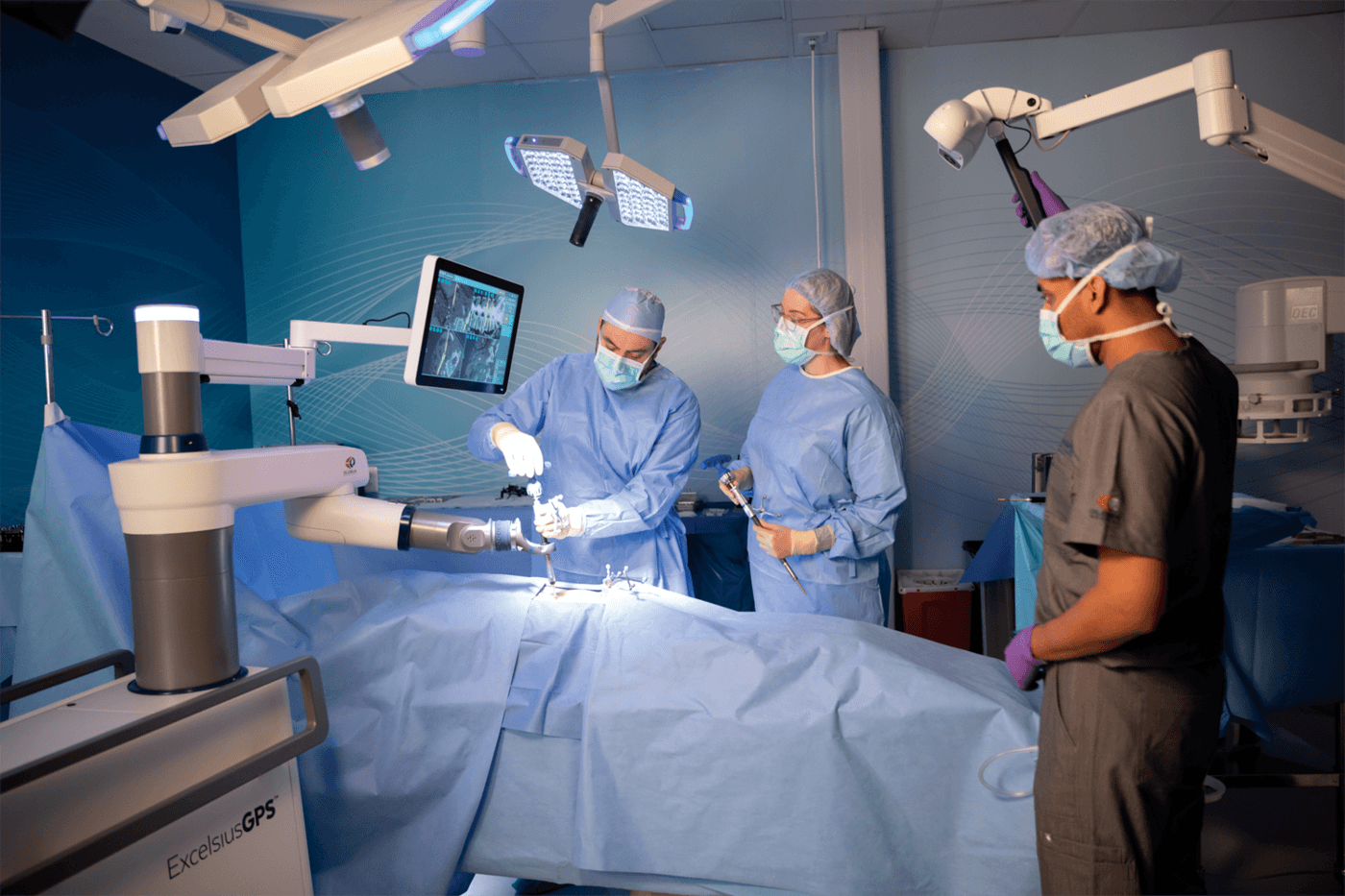
The use of robotics and robotic surgery has long been the stuff of science fiction media; but no longer. The image of the futuristic lab coated scientist and his metallic aide have been put to rest, with innovations within the robotic field now expanding into patient care. However, behind every brand new flatscreen, interconnected and end effector assisted surgery there is a continuing battle. This is not just for the health and wellbeing of the patient, but also for the eternal search for value for money capital investment and cost efficiencies. The initial costs of robotic procedures can look high in comparison to traditional multiport laparoscopy and camera methodology. But, in terms of patient pre-op care and the sheer amount of labour-intensive patient preparation by more traditional methods of staffing, the costs of automating such surgical procedures can start to add up. What Are the Advantages? The good news is excellent improvement in patient recovery times mainly due to the nature of precision surgery. The use of robotic surgery has enhanced recovery times down to 4.9 days as opposed to 6.1 days for traditional Laparoscopic procedures - with parallel reductions in pain, tissue scarring and secondary infections. (1) The Use of Telepresence This is a term meaning using the technology as available for the remote viewing of patients and using the associated physical technology and hard-wired telecommunication connections. A surgeon could be an entire continent away if necessary, meaning distance and time critical procedures are no longer a barrier to any operating procedures. Always On Duty The good news is robots don’t get tired. A simple diet of electricity is usually all they need while the corresponding human surgical controller remains less stressed (once fed and rested, of course). Human error is much reduced along with second surgeries, once programming procedures for each specific medical casebook have been written into the robotic programming and the surgeon is trained and savvy with operating the robotic systems. They Make Great Assistants Robots now come in all shapes and sizes and can assist in distributing and restocking consumables such as drugs, dressings and forwarding administration work with the more advanced robotic models acting as mobile stretcher-bearers along pre-programmed routes within advanced hospital architecture. This can release nursing and auxiliary staff to have more quality time for care duties with their charges. It's not just the physical quality of the hardware that has been improving over the last three decades; we’ve seen dramatic improvements in the writing of instructions that have allowed a certain amount of human approved autonomy as the term A.I. or artificial intelligence has crept into the medical vocabulary. Increasingly, manufacturers are adapting or creating brand new software and hardware packages specifically with surgical needs in mind. Many established robotic manufacturers are collaborating with leading consultants to develop remote hands-on technologies that are providing added value by lowering costs of surgery in terms of added value. An increasing number of procurement managers are taking onboard the cost advantages, both long and short term, of robotic interactions between surgeons and patients. The data available from such tailored systems installed in hospital operating theatres allows the closer scrutiny of procedures in a tangible manner, which in turn can be analysed by accountants and clinical management for their cost benefits in a way hitherto inaccessible. This has led to financing of robotic assets to health authorities that have become known as pay per use and managed service solutions. The most popular simple analogy would be to liken use to a vehicle leasing scheme with all costs built into a maintenance contract. Both schemes offer planning for operation costs with the flexibility for future proofing technologies and no concerns about depreciation nor equipment disposal at end of contracts. As with any technology, medical science robotics is quite literally cutting-edge and is continually evolving. There is no reason why such innovative developments should not continue to benefit not just patients, but also provide cybernetic support as the surgeon and robotic assistant end effector surgical glove for the benefit of patients and staff involved in all stages of the surgical and recuperative procedure. At the time of completing this paper, fresh news has suggested that patient preparation time is actually increased. New studies highlight that the savings realised are post operative recovery and revision rates with all the robotic companies racing to establish robust evidence. One of the challenges for payers, notably within the implant market, is open-source software for proprietary robots to expand access and maintain competition for implant suppliers. The jury, therefore, is still out on robotics surgery with the payers raising red flags as new case studies are presented against training times, routine disruption, sustainability and the F.D.A. caution against its use for Cancer (2). (1) https://www.nationalhealthexecutive.com/articles/robotics-and-robotic-surgery-how-access-better-patient-care (2) https://www.medtechdive.com/news/as-robotic-surgery-booms-fda-cautions-against-use-for-cancer/549459/

By Charles Daniel McDonald
•
17 Nov, 2022
A new innovative oncology software has been successfully piloted at Newcastle Hospital’s NHS Foundation Trust, and is now set to be rolled out to 47 other specialist cancer centres across England. The initiative supports The National Cancer Programme of Care NHS England and Improvement Specialised Commissioning, who have invested £1.4m on a three-year programme of evaluation, supported by The National Institute for Health and Care Excellence. This aims to determine the quality benefits that innovation can bring to the treatment of cancer patients, in line with the NHS Long Term Plan. The software in question, which is available via the NHS Supply Chain's Large Diagnostic Capital Equipment (including Mobile and Services radiotherapy framework), was selected because of its capability to improve treatment plan quality and outcomes. It follows an extensive phase of provider testing that enabled more than 20 radiotherapy centres in England to access, test and assess the system using anonymised data. Newcastle Hospital’s NHS Foundation Trust has played an important role in trialling the software, which enables trusts to evaluate details with peers securely, sharing pathology reports, live videos and insights. The software can also be used to support local audits and improvements in treatment plan quality, and through its use, anonymised dosimetry data will form the basis of national comparative quality audits, in-line with the prescribed clinical priorities. Chris Walker, Head of Radiotherapy Physics Northern Cancer Care, Newcastle said: “The NHS constantly measures the quality of its services to ensure that patients get the best care. This software will massively reduce the amount of time it takes to do that, meaning clinicians can spend more time with patients at a time when they need it most.” This new software will allow oncologists to use the expertise outside of their own hospital, and ultimately expedite the process of treating patients, an asset which could combat some of the backlog the NHS is currently facing. Antonia Marks, Tower Director for NHS Supply Chain: Large Diagnostic Capital Equipment including Mobile and Services said: “We are pleased to have this innovative software solution available on our framework. By centralising data through software, NHS trusts can share best practice with other cancer centres in the UK, as well as providing improved patient care." NHS Supply Chain, which manages the sourcing, delivery and supply of healthcare products, services and food for NHS trusts and healthcare organisations across England and Wales, was said to be pivotal in the procurement of the software. One of their core business aims is to support NHS Trusts to deliver safe effective patient care. Call us for a confidential chat on how we can help you navigate NHS Supply Chain, Integrated Care Boards and NHS Trusts to deliver strategic customer solutions, cement relationships and future proof your business.

By Charles Daniel McDonald
•
17 Nov, 2022
During the unmitigated medical emergency that has continued worldwide over the last two years, it comes as no surprise to any medical health professional that growing the market for ‘Medical Technical’ solutions is becoming more demanding. The desire to work unhindered within an interesting and innovative technology sector with the hope of becoming a market innovator of new products isn’t easy; especially when everyone including those that are trying to get a foothold and be newly established in the industry is scrambling to fulfil existing needs. It’s becoming an unwelcome challenge on the minds of CEO’s already with, more than enough on their organisational plate. The rapid spread of COVID-19 brought the medical industrial complex responding to the call with an Apollo Programme-like zeal; not just for those companies that could afford it - but also for fledgling companies willing to take a gamble on their own research and development programs. As many CEO’S in all industries have learned to their cost over the years, it is all too easy to be blind-sided by the term ‘’Innovative’’, while throwing into the mix precious resources in the name of developing products deemed to be “feature-packed” albeit cars, gadgets or medical technology. In the scramble to get what often turns out to be a mere month or two advantage over competitors these days, the technological advantages of new medical developments become an arms race which is too frequently unacknowledged by the company P.R. department who at best may issue an A4 sheet of information aimed at jaded periodical copy editors and at worst may, be ignored completely by them. This is part of the reason marketing has become the strategy with an importance to be emphasised in today’s competitive world of business. Smart marketing and research of MedTech products in particular are just like any other. They need to be determined just what sort of services and price can be structured in support for a new product, both pre and post launch and also need accurate monitoring right through to the end of a products shelf-life alongside what if any improvements are needed to enhance and tweak its desirability. Such factors are more important than ever and especially important in a crowded and competitive post COVID-19 marketplace world. So, while we’re on a roll extolling the virtues of accurate market access marketing, let’s take a closer look at some of the factors that will make your new product more successful from the get-go.

By Colette Hamilton
•
10 Nov, 2022
So, you have great commitment from a surgeon/physician and you've provided them with a strong business case template to submit for approval. That's the best you can do, right? WRONG. In most cases the clinician championing the adoption of your technology is not the key decision maker holding the budget. The budget holder may not even be in the same department and the final decision may be four or more steps away from the budget holder. Think of the business case as if it were a surfboard. It can be made of the best materials, with great design and aesthetics, but without a great big wave beneath it, it's going nowhere. It's the same with a business case. All the right stakeholders need to be engaged to generate a great big wave of support behind the case. If your field sales team and product managers don't get this right, they will easily lose faith in all the great value communication tools you are handing their way, and they will soon be collecting dust on a shelf. Patients won't have access to the technologies they need, and you have a bunch of field activities going on that are not contributing anything to business growth.

By Colette Hamilton
•
31 Oct, 2022
The chances are, if a physician decides to adopt your new technology into their daily practice, they will first need to secure approval from a clinical governance oversight body and the relevant budget holders. To do this, they will need to submit their case for investment and evidence backed assurance that the technology in use is both safe and cost effective, compared to currently available treatment options. Collating supportive evidence and building the case is time consuming. Doctors may have neither the time and/nor expertise to do this themselves, and limited access to the right in-house support. For these reasons, MedTech industry marketeers sometimes create an off the shelf business case for doctors, to save them time and avoid multiple doctors having to reinvent the business case "wheel" across the healthcare system. However, because hospitals are cash limited, when budget pressures are high, many business cases are rejected or deprioritised and parked until the next round of funding round. There are many reasons for this, falling outside the scope of this post, but here we focus - on the quality of the business case itself and list the top 10 reasons why business cases fail: Business cases that have a low chance of success are characterised by a failure to: INSTIL TRUST - marketing departments treat the case as though it were a piece of marketing material and cover it in branding. This raises concerns about commercial bias for decision makers. ADDRESS THE RIGHT AUDIENCE - the case is made from the perspective of the supplier and the physician i.e., the technology user, instead of the stakeholder who will be making the decision. The case therefore fails to address what's in it for them if they invest. In building the case, the developer has failed to consider what keeps the decision makers awake at night, along with the behavioural incentives and disincentives which will impact on their decisions. PROVIDE ADEQUATE CONTEXT - context matters. For example, if the new technology addresses an area of high unmet need and there are no effective alternatives, or if the existing standard of care has very little evidence to substantiate it, other than "it has always been done this way", then the evidence supporting the case may be scrutinised through a different lense. INCLUDE ALL OPTIONS - economic decisions are all about balancing benefits and risks, based on understanding the that "if you do this" then "you can't do that". Decision makers expect a full appraisal of options for solving a particular healthcare challenge, including alternative drugs, devices, digital health products, combinations and the "do nothing" option. ADDRESS ORGANISATIONAL PRIORITIES - hospital providers operate within their own organisational ecosystem, with their own goals, objectives, pressures and cadence of decision cycles. They must also operate within externally imposed boundaries, such as laws, policies and contractual commitments. For example, if the hospital needs to free up theatre capacity to clear an elective waiting list backlog, then a case that focuses on surgical hand strain isn't going to hit the right chord compared with another that does. If the clinical director of the surgery unit is an upper GI surgeon and needs an electroporator, then it's likely to be prioritised over a business case for disposable instrument packs for gynaecology. ADDRESS HORIZONTAL IMPACT - decision makers need to understand the impact on costs, capacity and workflows across budget and organisational silos, including for support services, such as porters and patient transport and path lab services etc. ADDRESS LONGITUDUNAL IMPACT - decision makers need to understand the impact along and even beyond the patient's episode of care. Will the new technology have in impact on length of stay, readmissions within 30 days and emergency visits? ADDRESS COST IMPACT - when economic studies, or clinical studies with economic end points, are published, they invariably address the question of cost effectiveness or cost utility. However, whilst useful when comparing the relative merits of competing priorities, these don't address the financial impact for the hospital i.e., the impact on operating costs; income and financial flows across budget silos. These must usually be calculated or estimated for the purpose of the case, using a budget impact model. CONSIDER IMPLEMENTATION - in order to understand now benefits, risks and costs will change over time, a detailed implementation plan should be included with non-recurrent implementation costs, phased activity costs, timelines and discounting of benefits. COMMIT TO MONITORING & EVALUATION - essentially a business case is a commitment to deliver Y benefit for X investment. Without a plan to monitor if cost estimates were accurate, and benefits were delivered, the business case is incomplete. Of course, business cases that strongly address the above points have a high degree of success, subject to other conditions being met. See "Conditions to Meet to Unlock Investment by HCPs in New Technologies". It should also be noted that many hospitals have a proforma based system for submitting business cases so the case should be structured to allow easy cutting and pasting of content into the proforma. The business case and financial modelling methodology deployed by Imperetus has a 95% success rate across the EU.
Genesyze
The global MedTech market access sherpas. An Imperetus delivery partner.
| Services | ||
|---|---|---|
| ✓ Health Economics | ✓ Patient Engagement | ✓ Interim Staffing |
| ✓ Operational Research | ✓ Sales Training | ✓ Project Delivery |
| ✓ Health Outcomes Research | ✓ Value Comms | ✓ Planning |
CONTACT US
Address:
Monument
10 Lower Thames Street
Billingsgate
London
EC3R 6AF United Kingdom
Mail: impetus@imperetus.com
Phone: +44 208 087 2258
LET’S CONNECT
SEND A MESSAGE
Thank you for your message.
We will get back to you as soon as possible.
Oops, there was an error sending your message.
Please try again later or email us: impetus@imperetus.com. Thanks and apologies for the inconvenience.



